The State of Pelvic Floor Physical Therapy
– Wang B, Chen Y, Zhu X, et al. Global burden and trends of pelvic organ prolapse associated with aging women: An observational trend study from 1990 to 2019. Front Public Health. 2022;10:975829. Published 2022 Sep 15. doi:10.3389/fpubh.2022.975829
– Jakus-Waldman S, Brubaker L, Jelovsek JE, et al. Risk Factors for Surgical Failure and Worsening Pelvic Floor Symptoms Within 5 Years After Vaginal Prolapse Repair. Obstet Gynecol. 2020;136(5):933-941. doi:10.1097/AOG.0000000000004092
– Bradley SL, Weidner AC, Siddiqui NY, Gandhi MP, Wu JM. Shifts in national rates of inpatient prolapse surgery emphasize current coding inadequacies. Female Pelvic Med Reconstr Surg. 2011;17(4):204-208. doi:10.1097/SPV.0b013e3182254cf1
– Tayyeb M, Gupta V. Dyspareunia. [Updated 2023 Jun 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562159/
– Bedaiwy MA, Patterson B, Mahajan S. Prevalence of myofascial chronic pelvic pain and the effectiveness of pelvic floor physical therapy. J Reprod Med. 2013;58(11-12):504-510.
– Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50(17):1092-1096. doi:10.1136/bjsports-2016-096065
– Lee D, Hodges PW. Diastasis rectus abdominis – should we open or close the gap? Musculoskeletal Science and Practice. 2017;28. doi:10.1016/j.math.2016.10.042
– Melville JL, Katon W, Delaney K, Newton K. Urinary Incontinence in US Women: A Population-Based Study. Arch Intern Med. 2005;165(5):537–542. doi:10.1001/archinte.165.5.537
– Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10(10):CD005654. Published 2018 Oct 4. doi:10.1002/14651858.CD005654.pub4
– Coyne KS, Wein A, Nicholson S, Kvasz M, Chen CI, Milsom I. Economic burden of urgency urinary incontinence in the United States: a systematic review. J Manag Care Pharm. 2014;20(2):130-140. doi:10.18553/jmcp.2014.20.2.130
– Capel-Alcaraz AM, García-López H, Castro-Sánchez AM, Fernández-Sánchez M, Lara-Palomo IC. The Efficacy of Strength Exercises for Reducing the Symptoms of Menopause: A Systematic Review. Journal of Clinical Medicine. 2023; 12(2):548. https://doi.org/10.3390/jcm12020548
– Ignácio Antônio F, Herbert RD, Bø K, et al. Pelvic floor muscle training increases pelvic floor muscle strength more in post-menopausal women who are not using hormone therapy than in women who are using hormone therapy: a randomised trial [published correction appears in J Physiother. 2020 Jan;66(1):7-8]. J Physiother. 2018;64(3):166-171. doi:10.1016/j.jphys.2018.05.002
– Zhuo Z, Wang C, Yu H, Li J. The Relationship Between Pelvic Floor Function and Sexual Function in Perimenopausal Women. Sex Med. 2021;9(6):100441. doi:10.1016/j.esxm.2021.100441
– Grimes WR, Stratton M. Pelvic Floor Dysfunction. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559246/
– Smith CP. Male chronic pelvic pain: An update. Indian J Urol. 2016;32(1):34-39. doi:10.4103/0970-1591.173105
The State Of Pelvic Floor Physical Therapy
 If you’ve made it to our website, chances are you
have been researching, or have been referred to
pelvic floor physical therapy for some sort of pelvic
related dysfunction.
If you’ve made it to our website, chances are you
have been researching, or have been referred to
pelvic floor physical therapy for some sort of pelvic
related dysfunction.
While searching, you may have noticed that there is an overwhelming amount of information targeting pelvic floor dysfunction.
It can feel daunting (and we are here to help), but the increase of pelvic floor related content is a positive in the realm of healthcare!

 It is estimated that around 30% of US women and
16% of men suffer from some sort of pelvic floor
dysfunction. The burgeoning field of pelvic floor
therapy means more people seeking the care they
desperately need, but unfortunately interest does not
always translate to acquiring care.
It is estimated that around 30% of US women and
16% of men suffer from some sort of pelvic floor
dysfunction. The burgeoning field of pelvic floor
therapy means more people seeking the care they
desperately need, but unfortunately interest does not
always translate to acquiring care.Despite growth, there is still a large gap between providers and those who need pelvic floor focused care. There is no official registry of pelvic floor physical therapists, but it is estimated there are roughly 10,000 providers equipped to care for the estimated 40 million who need care (APTA).
40M
patients in need of treatment
10K
pelvic floor PT’s

 A quick search through registries and Google listings
for the entirety of Oklahoma, North Texas, Northwest
Arkansas, and Southeast Kansas shows fewer than
100 practitioners providing pelvic floor care. For
many patients, they are driving up to an hour to
access the care they need.
A quick search through registries and Google listings
for the entirety of Oklahoma, North Texas, Northwest
Arkansas, and Southeast Kansas shows fewer than
100 practitioners providing pelvic floor care. For
many patients, they are driving up to an hour to
access the care they need.
Practicing pelvic floor physical therapy requires extensive and costly training beyond the standard of most doctorate programs, which fosters patient inaccessibility and creates a barrier to practitioners pursuing pelvic floor PT.
Physical therapy programs and residencies are just now trying to catch up to demand, with much more work to do in order to see a significant change in provider to patient ratio.
 Aside from the lack of accessibility to training, there
is a compensation gap too. Reimbursement rates for
pelvic floor physical therapy are often unsustainable
for the clinic, and leave patients with surprise bills.
Aside from the lack of accessibility to training, there
is a compensation gap too. Reimbursement rates for
pelvic floor physical therapy are often unsustainable
for the clinic, and leave patients with surprise bills.
The constant back and forth with insurance and restrictions put on plan of care creates clinician burnout and low quality of care. All of these factors come together to create scarcity in first-rate treatment.
At Vitality, we have sought to go out of network to circumvent some of these issues, increasing our direct accessibility and providing premium care with no surprise medical bills.
Our patient’s typically see quick results on a shorter, more holistic plan of care that is highly tailored to their individual needs.
 What about other barriers to care? Knowledge of
care and knowledge of treatment in the general
population is still very low.
What about other barriers to care? Knowledge of
care and knowledge of treatment in the general
population is still very low.
Many individuals suffering from pelvic floor dysfunction have no idea this is an option for them, or lack the knowledge about what to expect as far as treatment protocols are concerned. (It’s not just kegels).
Women also commonly express feelings of shame, normative thinking, fear of judgment, and self-blame in regards to their pelvic floor dysfunction. We are here to tell you that your symptoms are not normal, are not your fault, are not shameful, and can absolutely be addressed.

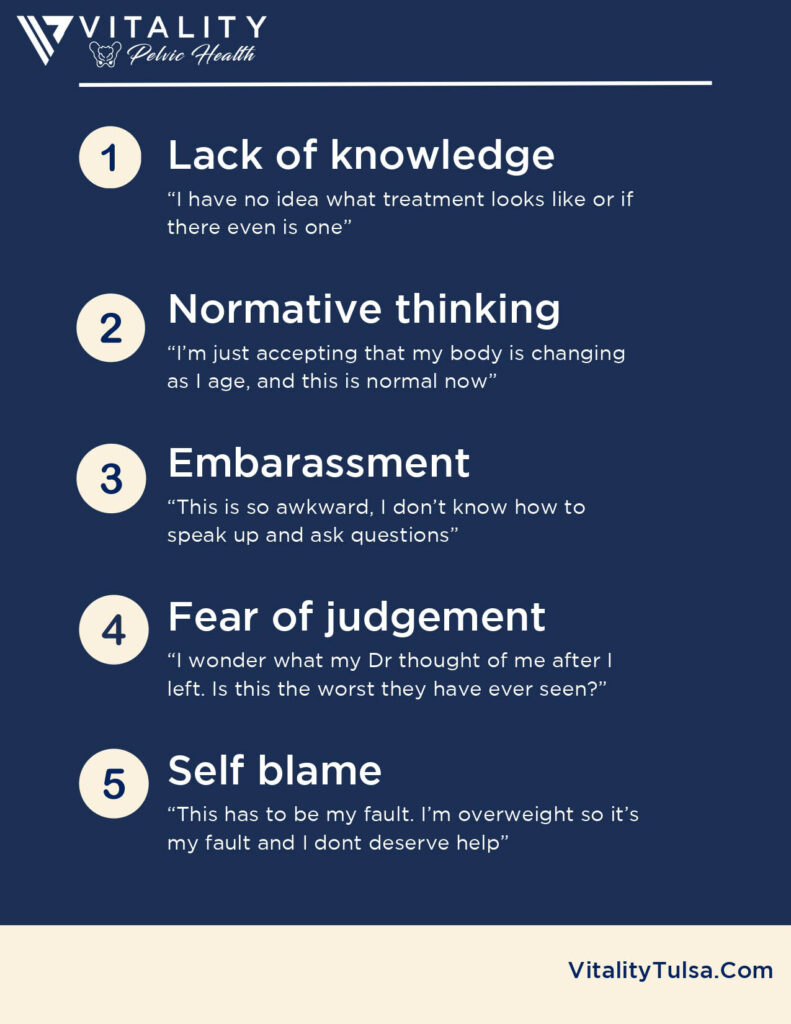
- Lack of knowledge “I have no idea what treatment looks like or if there even is one”
- Normative thinking “I’m just accepting that my body is changing as I age, and this is normal now”
- Embarassment “This is so awkward, I don’t know how to speak up and ask questions”
- Fear of judgement “I wonder what my Dr thought of me after I left. Is this the worst they have ever seen?”
- Self blame “This has to be my fault. I’m overweight so it’s my fault and I dont deserve help”
 Potential patients are not alone in this either, many
physicians do not understand the efficacy of pelvic
floor physical therapy and therefore are less likely to
refer.
Potential patients are not alone in this either, many
physicians do not understand the efficacy of pelvic
floor physical therapy and therefore are less likely to
refer.
Many programs in the US do not teach physicians full evaluation and diagnosis of musculoskeletal disorders from a functional standpoint, leaving them limited in what they can suggest to their patients.

If physicians know it’s needed, they may not know who to refer to in their community. Screening for pelvic floor dysfunction and referral to conservative care can eliminate unnecessary lab tests, imaging, and financial burden.
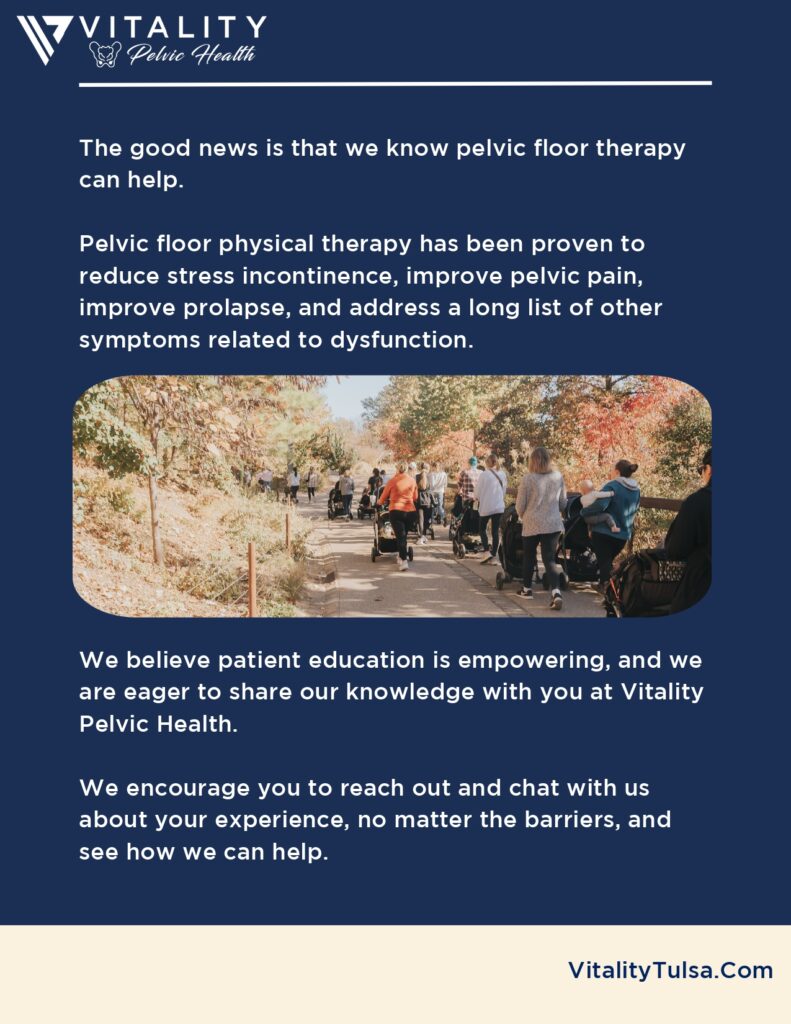
 The good news is that we know pelvic floor therapy
can help.
The good news is that we know pelvic floor therapy
can help.
Pelvic floor physical therapy has been proven to reduce stress incontinence, improve pelvic pain, improve prolapse, and address a long list of other symptoms related to dysfunction.

We believe patient education is empowering, and we are eager to share our knowledge with you at Vitality Pelvic Health.
We encourage you to reach out and chat with us about your experience, no matter the barriers, and see how we can help.