Hip and pelvic pain refers to discomfort experienced in the hip joints and the surrounding pelvic region, which can range from mild to severe and may be associated with a variety of underlying conditions. This type of pain is quite prevalent, affecting individuals of all ages, and it can significantly disrupt daily activities, limiting mobility and reducing overall quality of life. Recognizing and understanding the causes and symptoms of hip and pelvic pain is essential for effective management. Gaining insight into the factors contributing to this discomfort can lead to appropriate treatments and preventive measures, ultimately enhancing well-being. In this article, we will explore the anatomy of the hip and pelvis, explore common causes of pain, examine associated symptoms, discuss diagnostic processes, and review treatment options, along with strategies for prevention.
Anatomy of the Hip and Pelvic
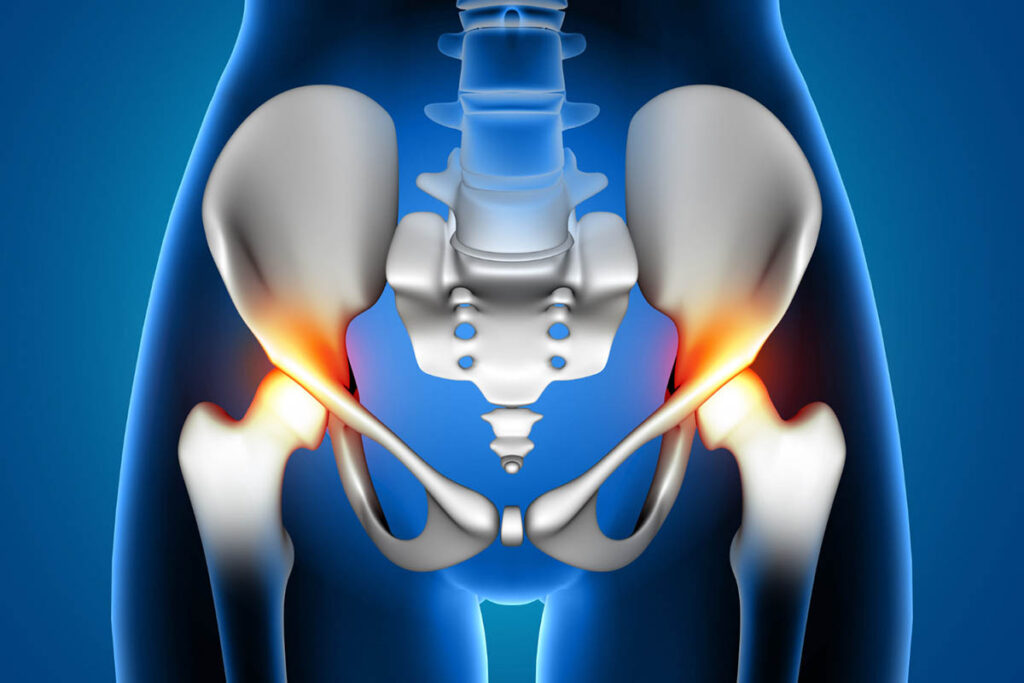
To understand hip and pelvic pain, it’s essential to know the anatomy involved. The hip joint is a ball-and-socket joint where the head of the femur (thigh bone) fits into the acetabulum of the pelvis. This joint allows a wide range of motion and bears the weight of the body during various activities. The pelvis, located at the base of the spine, supports the spine and connects the trunk to the lower limbs. It comprises the sacrum, coccyx, and two hip bones (ilium, ischium, and pubis). The pelvic region is also home to several vital structures, including nerves, blood vessels, and muscles. This region plays a crucial role in supporting the pelvis and connecting it to the hip, which can lead to pelvic floor and hip pain. The pelvic bones form the foundation for the pelvic girdle and play a crucial role in supporting the upper body and transferring weight to the lower limbs.
Common Causes of Hip and Pelvic Pain
Hip and pelvic pain can arise from various underlying conditions, such as arthritis, tendonitis, bursitis, fractures, or injuries. Additionally, issues related to the lower back, hip labral tears, and even certain infections can contribute to the discomfort experienced in these areas.
Hip Pain
Hip pain can stem from a variety of factors, including degenerative conditions, injuries, or structural abnormalities in the joint. In a published study, 14.3% of adults reported significant hip pain on most days over the previous six weeks. For instance, hip pain athletes may experience discomfort due to overuse or sports-related injuries. Conditions such as hip fracture, bursitis, hip labral tears, and tendonitis are common contributors. Hip arthritis involves the degeneration of cartilage in the hip joint, which can lead to intense pain, stiffness, and decreased mobility over time.
Hip Fracture
A hip fracture is a break in the upper part of the femur, often caused by trauma or falls, particularly in older adults with weakened bones. This condition results in severe pain, difficulty moving the hip, and inability to bear weight.
Bursitis
Hip bursitis involves inflammation of the bursa, a fluid-filled sac that cushions the hip joint. It can result from repetitive stress or direct trauma, causing pain and tenderness on the outer side of the hip.
Hip Labral Tears
The labrum is a ring of cartilage that surrounds the hip socket, providing stability and cushioning. Tears in the labrum can occur due to injury or degeneration, leading to pain, stiffness, and a sensation of catching or locking in the joint.
Tendonitis
Tendonitis refers to inflammation of the tendons around the hip joint, often caused by overuse or repetitive stress. Symptoms include pain, swelling, and reduced range of motion.
Hip Arthritis
Worldwide, the number of people suffering from arthritis is approximately 355 million, including more than 151 million with osteoarthritis (OA). In the US alone, about 10 million people have reported a diagnosis of osteoarthritis of the hip. Hip arthritis involves the degeneration of cartilage in the hip joint. This condition leads to pain, stiffness, and decreased mobility over time.
Pelvic Pain

Pelvic pain can arise from various underlying conditions, including infections, diseases of the reproductive organs, or dysfunction of the musculoskeletal system. Chronic pelvic pain (CPP) affects up to 25% of females of reproductive age and 15% of all females worldwide. Understanding the specific cause of pelvic hip pain is crucial for effective treatment and management of symptoms.
Pregnancy
Pregnancy can cause pelvic pain after birth due to the hormonal changes that relax the ligaments and the additional weight and pressure on the pelvis. This type of pain often subsides after childbirth but may require management during pregnancy.
Pelvic Injury
Pelvic injuries, such as fractures or trauma from accidents, can lead to significant pain and discomfort in the pelvic region.
Gout
Gout is a type of arthritis caused by the buildup of uric acid crystals in the joints, including the pelvis. It results in sudden, severe pain and swelling.
Walking Patterns
Abnormal walking patterns or gait can contribute to pelvic pain by placing undue stress on the pelvic region and surrounding muscles.
Ankylosing Spondylitis
Ankylosing spondylitis is a type of inflammatory arthritis that primarily affects the spine and pelvis, leading to pain, stiffness, and reduced flexibility.
Osteoarthritis
Osteoarthritis of the pelvis involves the degeneration of cartilage and can cause pain, stiffness, and impaired movement.
Symptoms of Hip and Pelvic Pain
Hip and pelvic pain can present itself in several forms, such as a dull ache or sharp pain localized in the hip or pelvic region. You may notice that the pain intensifies with movement or when putting weight on the affected area. Additionally, hip and pelvic pain when walking can occur, often accompanied by stiffness, a decrease in range of motion, and swelling or tenderness in the vicinity. Often, this pain can extend, radiating toward the groin, upper thigh, or lower back, complicating the overall discomfort experienced. Pain at night or pain during intercourse is also common, especially if related to chronic conditions or soft tissue injuries.
Diagnosis of Hip and Pelvic Pain
To diagnose hip and pelvic pain, a healthcare provider will typically conduct a comprehensive physical examination and review the patient’s medical history. Diagnostic imaging, such as X-rays or MRIs, may also be utilized to identify underlying causes and guide treatment options.
Physical Examination
A thorough physical exam helps assess range of motion, tenderness, and areas of pain. It also evaluates how the pain affects movement and daily activities. During the pelvic exam, the provider may assess the pelvic organs and pelvic floor muscles.
Medical History Review
Reviewing the patient’s medical history provides insights into potential causes, such as previous injuries, medical conditions, or activities that may contribute to pain. This includes assessing previous surgery, chronic conditions, and health issues related to hip muscles.
Imaging Tests
Imaging tests, such as X-rays, MRI, or CT scans, help visualize the structures within the hip and pelvis. These tests can reveal fractures, tears, arthritis, or other abnormalities. Blood tests may also be conducted to rule out bacterial infections or other health conditions.
Treatment Options for Hip and Pelvic Pain
Effective treatment for hip and pelvic pain often includes a combination of physical therapy, medication, and lifestyle modifications to alleviate symptoms and improve function. In more severe cases, surgical interventions may be considered to address underlying conditions contributing to the pain.
Non-surgical Treatment
Non-surgical treatments for hip and pelvic pain typically involve physical therapy Tulsa, medications, and lifestyle changes aimed at reducing symptoms and enhancing mobility. These approaches are often the first line of defense before considering more invasive options.
- Rest: Allowing time for the affected area to rest and heal can alleviate pain and prevent further injury.
- Applying Ice: Ice packs can reduce inflammation and numb the affected area, providing temporary relief from pain.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs, such as ibuprofen or aspirin, can help reduce pain and inflammation.
- Massage: Therapeutic massage can relieve muscle tension and improve circulation, helping to ease pain and promote healing.
- Corticosteroid Injections: These injections can reduce inflammation and provide temporary relief for conditions like bursitis or arthritis.
- Physical Therapy: A physical therapist can design a customized exercise program to strengthen the muscles around the hip and pelvis, improve flexibility, and alleviate pain.
Surgical Treatment for Severe Cases
When non-surgical treatments fail to provide relief for severe cases, surgical interventions may become necessary. Options include hip arthroscopy, joint replacement, or pelvic surgery to address the underlying issues causing pain.
Prevention Strategy to Avoid Hip and Pelvic Pain

To effectively prevent hip and pelvic pain, it is essential to adopt several key strategies. First, maintaining a healthy weight can significantly reduce stress on the joints. Regular exercise is also crucial, as it strengthens the muscles surrounding the hips and pelvis while enhancing flexibility. Additionally, using proper techniques and appropriate equipment during physical activities helps minimize injuries. It is important to avoid repetitive stress and overuse, which can lead to discomfort, and to practice good posture and ergonomics in daily activities to support overall joint health.
For Hip and Pelvic Pain Relief, Consult Vitality Therapy & Performance
At Vitality Therapy & Performance, we offer comprehensive assessments and personalized treatment plans for hip and pelvic pain. Our experienced team can help you manage your pain and improve your quality of life through effective therapies and interventions.
Conclusion
Understanding the causes and symptoms of hip and pelvic pain is essential for effective management and treatment. Whether the pain is due to an injury, arthritis, or other conditions, early intervention and proper care can help alleviate the pain and improve mobility. Consult with healthcare professionals to determine the best course of action for your specific situation.
FAQ’S
How do you know if something is wrong with your pelvis?
Signs of a potential pelvic issue include persistent pain, discomfort while sitting or moving, swelling, and difficulty with mobility. If you experience these symptoms, it is essential to seek medical evaluation for a proper diagnosis.
Should I be worried about pelvic pain?
Pelvic pain can range from mild to severe and may indicate underlying issues. If the pain is persistent, worsening, or accompanied by other symptoms, it is crucial to consult a healthcare professional for evaluation and appropriate treatment.
When to worry about hip pain?
You should be concerned about hip pain if it is severe, persistent, or affects your daily activities. Additional red flags include significant swelling, inability to bear weight, or pain that radiates to other areas. Consult a healthcare provider for a thorough assessment and treatment options.