Autoimmune digestive disorders are a group of conditions where the immune system mistakenly attacks the gastrointestinal tract, causing inflammation, damage, and disruption to normal digestion. These disorders, such as Crohn’s disease, celiac disease, and autoimmune gastritis, are increasingly prevalent and have a profound impact on gut health. Understanding the interplay between the immune system and the digestive system is critical, as it provides insight into how to manage these conditions effectively.
The digestive tract is not only responsible for nutrient absorption but also serves as a significant hub for immune activity. Any disruption in this delicate balance can result in autoimmune gastrointestinal diseases, which affect not just the gut but overall health.
What Are Autoimmune Digestive Disorders?
Autoimmune digestive disorders involve an abnormal immune response targeting components of the digestive system, including the intestinal lining, parietal cells in the stomach, and other tissues. These conditions are influenced by genetic variations, environmental factors, dietary habits, and the gut microbiota. There are currently over 80 recognized autoimmune diseases, collectively affecting roughly 5–8% of the global population. These conditions represent a significant portion of chronic illnesses worldwide, underlining the need for greater awareness and research into their causes and treatments.
Some of the most common autoimmune gastrointestinal diseases include inflammatory bowel disease (IBD), which encompasses Crohn’s disease and ulcerative colitis, both of which involve chronic inflammation of the gastrointestinal tract. Celiac disease, another prevalent condition, is triggered by an immune reaction to gluten, causing damage to the small intestine. Autoimmune gastritis leads to inflammation of the stomach lining and hypochlorhydria, impairing digestion and nutrient absorption. Lastly, microscopic colitis is characterized by chronic inflammation of the colon, often causing persistent diarrhea and abdominal discomfort.
How Autoimmune Digestive Disorders Affect the Gut
Autoimmune digestive disorders disrupt gut function through chronic inflammation, immune dysregulation, and damage to the gastrointestinal tract. These conditions can affect the gut’s ability to absorb nutrients, maintain immune tolerance, and regulate digestion. Let’s explore how these disorders manifest.
Inflammatory Bowel Disease (IBD)
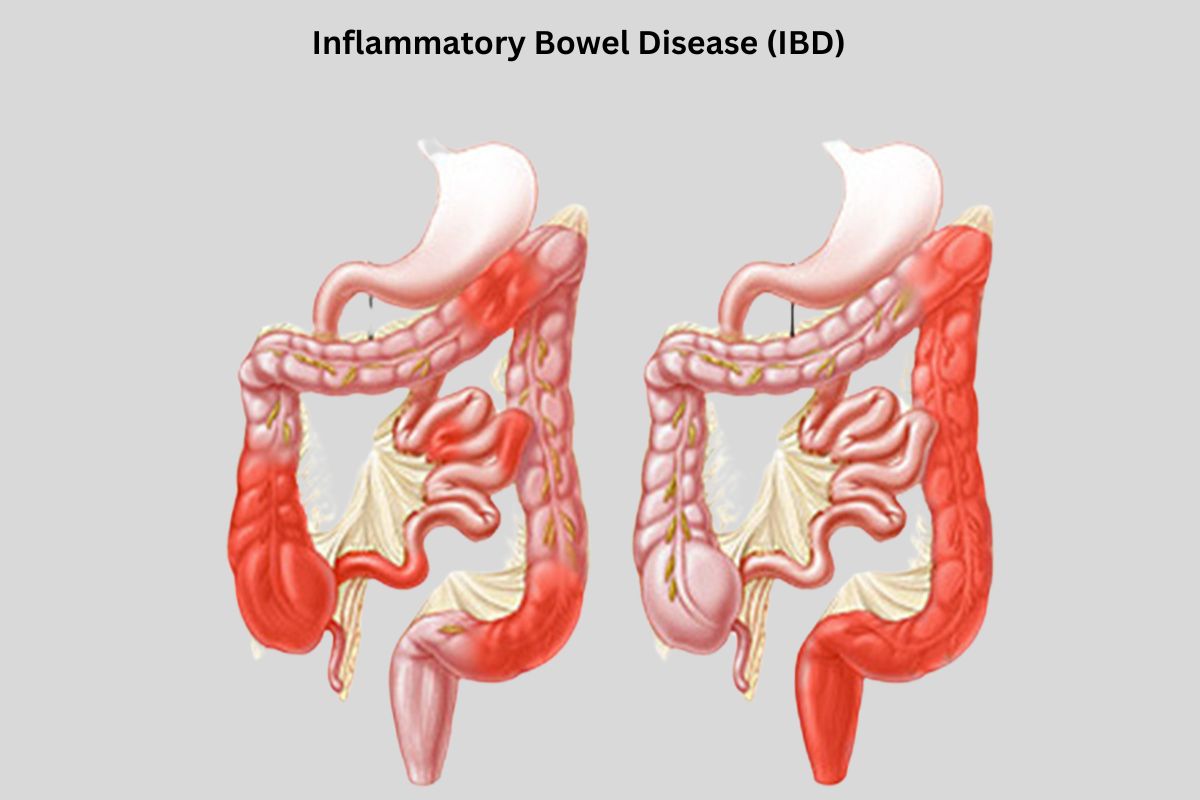
IBD is a broad term that includes Crohn’s disease and ulcerative colitis. Both conditions involve autoimmune inflammation of the gastrointestinal tract and can lead to significant digestive issues. Symptoms such as abdominal pain, diarrhea, and autoimmune disease stomach bloating are common, often affecting a patient’s overall quality of life and requiring comprehensive management strategies.
Crohn’s Disease
Crohn’s disease can affect any part of the digestive tract, causing deep inflammation that can lead to digestive tract motility issues such as subacute GI dysmotility. This inflammation may penetrate all layers of the intestinal lining, leading to complications like strictures, fistulas, and abscesses. Symptoms include abdominal pain, chronic diarrhea, weight loss, and systemic signs like muscle weakness and joint pain.
Ulcerative Colitis
Ulcerative colitis primarily affects the colon and rectum, causing ulcers and inflammation in the mucosal layer. This condition often leads to gastrointestinal manifestations like chronic diarrhea and blood in the stool. Severe cases may require surgical interventions such as a total colectomy.
Celiac Disease
Celiac disease is triggered by gluten, causing an autoimmune attack on the small intestine’s intestinal lining. This leads to villous atrophy, which impairs nutrient absorption and causes symptoms such as chronic diarrhea, bloating, and fatigue. A strict gluten-free diet is the primary treatment, helping to restore gut health and promote remission.
Autoimmune Gastritis
Autoimmune gastritis is characterized by antibodies to parietal cells and intrinsic factor, resulting in hypochlorhydria and impaired vitamin B12 absorption. Over time, this condition can progress to autoimmune metaplastic atrophic gastritis and gastric intestinal metaplasia, increasing the risk of gastric adenocarcinoma. Symptoms include stomach bloating, fatigue, and pernicious anemia, which often requires parenteral vitamin B12 for treatment.
Microscopic Colitis
Microscopic colitis involves inflammation of the colon, often diagnosed through endoscopy and biopsy. It is linked to autoimmune gastrointestinal dysmotility and typically causes chronic watery diarrhea and abdominal pain. Environmental factors, such as medications, may exacerbate the condition.
Irritable Bowel Syndrome (IBS)
While IBS is not strictly autoimmune, it is often associated with immune dysregulation. Symptoms include abdominal cramping, altered bowel habits, and bloating. Functional medicine approaches, such as stress management and dietary modifications, can improve symptoms. Irritable Bowel Syndrome (IBS) impacts an estimated 25 to 45 million individuals in the United States alone. Interestingly, the condition disproportionately affects women, with two-thirds of sufferers being female, while one-third are male. This gender disparity has prompted ongoing research into hormonal and physiological factors linked to IBS.
Common Symptoms of Autoimmune Digestive Disorders
Symptoms of autoimmune gastrointestinal diseases vary but often include:
- Abdominal pain and cramping – Caused by inflammation and digestive tract motility issues.
- Chronic diarrhea or constipation – Common in IBD, microscopic colitis, and celiac disease.
- Bloating and gas – Linked to autoimmune stomach issues and gluten intolerance.
- Fatigue and weakness – Often due to nutrient deficiencies from malabsorption.
- Unexplained weight loss – Common in Crohn’s disease and severe cases of celiac disease.
- Malabsorption – Causes deficiencies in iron, calcium, and B12, leading to pernicious anemia and muscle weakness.
Managing Autoimmune Digestive Disorders for Gut Health
Effectively managing autoimmune digestive disorders requires a comprehensive approach that addresses inflammation, restores immune balance, and supports gut function. This involves making targeted lifestyle changes, adhering to prescribed treatments, and exploring holistic approaches like functional medicine to maintain optimal gut health. By implementing these strategies, individuals can reduce symptoms, prevent flare-ups, and improve their overall quality of life.
Dietary Changes
Adjusting dietary habits can significantly improve gut health. A gluten-free diet is essential for celiac disease, while low-FODMAP or anti-inflammatory diets can alleviate symptoms in IBS and IBD.
Food Intolerance Testing
Testing for food intolerances helps identify triggers that exacerbate inflammation or cause gastrointestinal manifestations like bloating and diarrhea. This supports a more tailored dietary approach.
Take Medication as Prescribed

Medications such as immunosuppressants, biologics, and anti-inflammatory medication are essential for reducing inflammation and achieving remission. For autoimmune gastritis, intravenous immunoglobulin or insulin therapy may be required in specific cases.
Stress Management
Stress can worsen dysautonomia and gastrointestinal hypo- or hypermobility. Techniques like mindfulness, yoga, and cognitive-behavioral therapy support regulatory mechanisms in the gut-brain axis.
Functional Medicine
Functional medicine offers a holistic approach by addressing the root causes of autoimmune inflammation. This may include assessing gut microbiota, improving immune tolerance, and targeting cellular and molecular signaling pathways.
When to See a Doctor
Seek medical advice if you experience persistent symptoms like chronic diarrhea, severe abdominal pain, or unexplained weight loss. A gastroenterologist may perform blood tests, endoscopy, or GI transit studies to diagnose conditions and rule out differential diagnoses such as generalized autonomic syndrome or paraneoplastic conditions.
Conclusion
Understanding the link between autoimmune diseases and gut health is essential for managing these complex conditions. By recognizing symptoms early and adopting a well-rounded treatment plan, individuals can take control of their health and minimize the impact of autoimmune digestive disorders. Ongoing research and awareness will continue to shed light on effective treatments and strategies for living well with these conditions.
FAQs
What autoimmune disease affects the digestive system?
Autoimmune digestive disorders, including Crohn’s disease, celiac disease, and autoimmune gastritis, are common conditions that attack the digestive system.
What are the symptoms of stomach autoimmune diseases?
Symptoms of autoimmune stomach issues include stomach bloating, chronic diarrhea, fatigue, nutrient deficiencies, and pain.
Are probiotics good for autoimmune disease?
Probiotics can support gut microbiota and reduce inflammation. However, their use should be guided by a healthcare provider to ensure compatibility with autoimmune gastrointestinal diseases.

