Pelvic floor dysfunction, encompassing both hypotonic and hypertonic pelvic floor conditions, can significantly impact daily life, causing issues ranging from urinary incontinence to pelvic pain. The pelvic floor, a network of muscle groups in the pelvic region, plays a vital role in supporting the bladder, bowel, and reproductive organs. If the pelvic muscles are either too weak or too tight, it can result in uncomfortable or debilitating symptoms. Understanding the key differences between hypotonic vs hypertonic pelvic floor conditions is crucial to identifying appropriate treatment options. In this blog, we’ll explore how these dysfunctions manifest, their impact on daily life, and how to address them effectively.
What is the Pelvic Floor?
The pelvic floor consists of several muscle groups that stretch across the base of the pelvis, forming a supportive sling for the pelvic organs. This muscular structure helps maintain bladder control, assists in bowel movements, and plays a role in sexual function. Whether too strong or too weak, these muscles are prone to dysfunction, often leading to incontinence symptoms and other issues. These dysfunctions affect people of all ages and genders, sometimes as a result of childbirth, aging, or surgery (such as prostate surgery). Maintaining a balance in muscle tone is crucial to preventing problems.
Hypotonic vs Hypertonic Pelvic Floor: What’s the Difference?
The difference between a hypertonic vs hypotonic pelvic floor lies in the muscle tone of the pelvic muscles. A hypotonic pelvic floor refers to pelvic floor weakness, where the muscles lack sufficient strength or muscle tone to support the organs properly. In contrast, a hypertonic pelvic floor is characterized by pelvic floor tightness, where the muscles are overly tense or contracted. The weak vs tight pelvic floor debate highlights the fact that the symptoms and treatment for each condition differ significantly.
What is Hypotonic Pelvic Floor Dysfunction?
Hypertonic pelvic floor dysfunction occurs when the muscles in the pelvic region become excessively tight or overactive, leading to pain and difficulty in normal pelvic functions like urination, defecation, or sexual activity. This condition prevents the muscles from properly relaxing, which can cause chronic discomfort, bladder issues, and painful intercourse. Individuals with hypertonic pelvic floor often experience symptoms such as chronic pelvic pain, vaginismus, and difficulty with bladder and bowel control
Urinary Incontinence
A common sign of hypotonic pelvic floor dysfunction is urinary incontinence, where the inability to control bladder function leads to unintentional urine leakage. This condition can manifest in several forms:
Types of Urinary Incontinence:
- Stress incontinence: Occurs when pressure on the bladder, from activities like coughing, sneezing, or lifting, causes urine leakage. This happens because the pelvic muscles lack the strength to support the bladder effectively.
- Urge incontinence: Characterized by a sudden, intense urge to urinate followed by an involuntary loss of urine. It often coexists with bladder irritants or conditions like interstitial cystitis or irritable bowel syndrome (IBS).
- Overflow incontinence: Happens when the bladder doesn’t fully empty, leading to continuous urine leakage. This often results from weak bladder muscles or nerve damage.
- Mixed incontinence: Combines both stress and urge incontinence, affecting many individuals who suffer from multiple triggers.
Pelvic Organ Prolapse (POP)
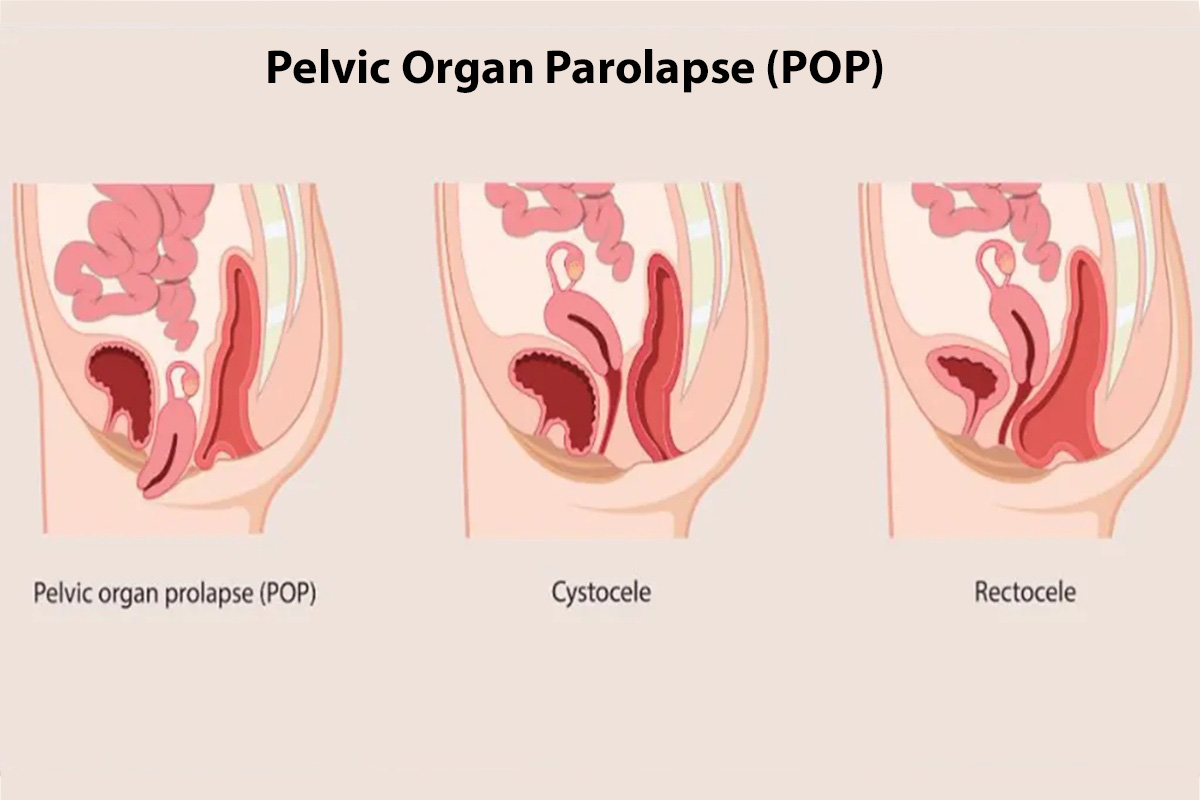
Pelvic organ prolapse occurs when weakened pelvic muscles can no longer support the pelvic floor organs, causing them to descend into the vaginal area. This can lead to sensations of pressure or bulging in the pelvic region and may cause discomfort during daily activities, including exercise or prolonged standing.
By the age of 80, approximately 11% of women will undergo one or more surgical procedures to address urinary incontinence or pelvic organ prolapse. This highlights how common these issues are and the potential need for surgical intervention in severe cases.
Sexual Dysfunction
Weakness in the pelvic floor can also lead to sexual dysfunction, affecting both physical and emotional aspects of a sexual encounter. Individuals may experience reduced sensation, difficulty achieving orgasm, or discomfort during intercourse. Addressing pelvic floor weakness can significantly improve both sexual functioning and confidence.
What is Hypertonic Pelvic Floor Dysfunction?
Hypertonic pelvic floor dysfunction, also known as Pelvic Floor Hypertonia, occurs when the muscles in the pelvic region become excessively tight or overactive, leading to pain and difficulty in normal pelvic functions like urination, defecation, or sexual activity. This condition prevents the muscles from properly relaxing, which can cause chronic discomfort, bladder issues, and painful intercourse. Individuals with hypertonic pelvic floor often experience symptoms such as chronic pelvic pain, vaginismus, and difficulty with bladder and bowel control.
It has been found that 60–90% of women experiencing chronic pelvic pain also suffer from high-tone pelvic floor dysfunction. This association underscores the need for a proper diagnosis, as addressing pelvic floor tightness can significantly improve quality of life.
Dyspareunia
Painful intercourse, or dyspareunia, is a hallmark of hypertonic pelvic floor dysfunction. The overactive muscles in the pelvic region make penetration painful, leading to discomfort during or after sex. This pain may affect the quality of intimate relationships and emotional well-being.
Vaginismus
Vaginismus occurs when involuntary tightening of the pelvic muscles makes penetration difficult or impossible. This condition is frequently associated with hypertonic pelvic floor dysfunction and can cause anxiety surrounding sexual activity.
Vulvodynia
Vulvodynia refers to chronic pain or discomfort in the vulvar area, often related to pelvic floor tightness. Individuals with vulvodynia may experience burning, stinging, or irritation without an obvious cause, often making diagnosis and treatment difficult.
Chronic Pelvic Pain Syndrome
Chronic pelvic pain syndrome is another symptom linked to a hypertonic pelvic floor. Persistent pelvic pain can limit daily activities, such as sitting, standing, or walking, and may require comprehensive treatment involving pelvic pain relief strategies.
Why is it Important to Know the Difference?
Understanding the differences between hypotonic vs hypertonic pelvic floor dysfunction is critical to finding the appropriate treatment. Treating a weak pelvic floor with kegel exercises can help strengthen the muscles and improve bladder control, while a hypertonic pelvic floor often requires down training and manual stretches to relieve muscle tension. Misidentifying the condition can result in ineffective treatments and potentially worsen symptoms.
In fact, research has revealed that a significant proportion of women—around 32%—are diagnosed with pelvic floor disorders, even if they are not actively seeking medical treatment. This suggests that many individuals may be living with undiagnosed symptoms, further highlighting the importance of early identification and treatment.
How Does Each Affect Daily Function?
Both hypotonic and hypertonic pelvic floor conditions can severely disrupt daily life. Hypotonic pelvic floor dysfunction may lead to incontinence symptoms, such as urinary incontinence and pelvic floor prolapse, while hypertonic dysfunction causes pelvic pain and difficulty during intercourse. Both conditions can limit physical activity, make social interactions uncomfortable, and reduce overall quality of life.
How Can Physical Therapy Help?

Working with a pelvic floor physical therapist is often the most effective approach to treating both hypotonic and hypertonic pelvic floor dysfunction. Therapists use techniques such as breathing exercises, core strengthening exercises, and kegel exercises to address pelvic floor weakness. For hypertonic pelvic floor dysfunction, therapies may include manual stretches, down training, and breathing exercises aimed at relaxing the muscles. Additionally, a bladder diary may help track symptoms and identify potential bladder irritants.
At Vitality Therapy and Performance, we provide expert, personalized care for pelvic floor dysfunction, including hypertonia and hypotonia. Our specialized therapy programs combine manual therapy, exercises, and lifestyle guidance to help you relieve pain, restore strength, and enhance your quality of life. Speak with PT today and take the first step toward better pelvic health.
What Are Other Treatment Options?
In addition to physical therapy, several other treatments can help manage pelvic floor dysfunction. Medications such as muscle relaxants or pain relievers may be prescribed to address conditions like pudendal neuralgia or interstitial cystitis. Surgical interventions may be necessary in more severe cases, such as pelvic organ prolapse, to provide structural support. Additionally, lifestyle modifications such as avoiding bladder irritants, practicing breathing exercises, and managing weight can alleviate symptoms and enhance overall pelvic health.
- Medications: For hypertonic pelvic floor dysfunction, muscle relaxants or pain relief medications may be prescribed, especially for conditions like interstitial cystitis or pudendal neuralgia.
- Surgical options: For more severe cases, such as pelvic organ prolapse, surgery may be necessary to provide structural support.
- Lifestyle modifications: Changes in diet, avoiding bladder irritants, and maintaining a healthy weight can improve symptoms.
High Tone or Low Tone, Whatever. How Do I Deal With It?
Whether your pelvic floor is too strong or too weak, the key to managing the symptoms lies in seeking expert care. A pelvic floor therapist can help you determine whether you have a hypotonic or hypertonic pelvic floor, and offer personalized treatment plans, including pelvic pain relief, kegel exercises, and manual stretches. Ignoring the symptoms can lead to worsening discomfort, but addressing the issue early can significantly improve your quality of life.
Conclusion
Pelvic floor dysfunction, whether caused by hypotonicity or pelvic floor tightness, can greatly impact both physical and emotional well-being. By identifying the strong vs weak pelvic floor conditions and seeking appropriate treatment, individuals can regain control of their pelvic health and daily function. With help from a pelvic floor therapist and other healthcare providers, you can reduce symptoms and improve your quality of life.
FAQs
How can I tell if I have hypertonic or hypotonic pelvic floor dysfunction?
Symptoms such as urinary incontinence, stool leakage, and pelvic organ prolapse typically suggest hypotonic pelvic floor dysfunction. On the other hand, pelvic pain, painful urination, and difficulty during intercourse are common with hypertonic pelvic floor dysfunction. A healthcare provider or pelvic floor therapist can perform an assessment to confirm the diagnosis.
Can pelvic floor dysfunction cause digestive problems?
Yes, both hypotonic and hypertonic pelvic floor dysfunction can affect bowel movements. Weak muscles may lead to constipation, while tight muscles can make passing stool painful. Conditions such as irritable bowel syndrome (IBS) can also be associated with pelvic floor dysfunction.
What is the role of physical therapy in treating pelvic floor issues?
Pelvic floor physical therapy plays a key role in treating both hypotonic and hypertonic pelvic floor dysfunction. A therapist can help strengthen weak muscles with kegel exercises or relax tight muscles with manual stretches and down training techniques.

